Did you know that every year we lose 14,000 women to cervical cancer? And although we have PAP screenings, which can detect abnormal cells, the number of deaths is staggering. You may be asking, what's the reason? Unfortunately, many women aren't getting regular screens and when cancer is finally detected, it's often too late.
Listen to this episode with Dr. Richard Conlen, OBGYN share his advice on how women can get in tune with and take care of their bodies. Dr. Conlen expands on everything from chronic conditions, to preventative care as well as covers what to do when you are looking to get pregnant. He also explains what the pelvic floor is and how to take care of it, along with learning what to be aware of when it comes to vaginal bacteria.
Key Takeaways
- Why and when you should get screened for HPV
- The importance of hormone health
- Get to know what the pelvic floor is and how it works
Hit play and learn all there is to know about what is optimal for women's health. Learn what you can do to take your health into your own hands.
Check out our podcast selection for valuable info on health, wellness, and more.
Continue the conversation in the Hero Moms Social Group on Facebook!
Connect with Checkable Health:
Facebook
LinkedIn
Connect with Patty Post:
https://www.linkedin.com/in/patty-post/
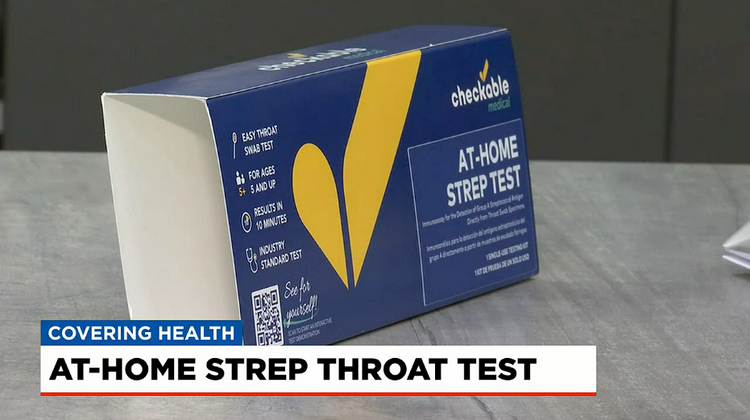
About Checkable
Checkable is revolutionizing healthcare with fast and accurate at-home test kits, telehealth services, and a line of wellness supplements designed to keep you feeling your best while saving valuable time and money.
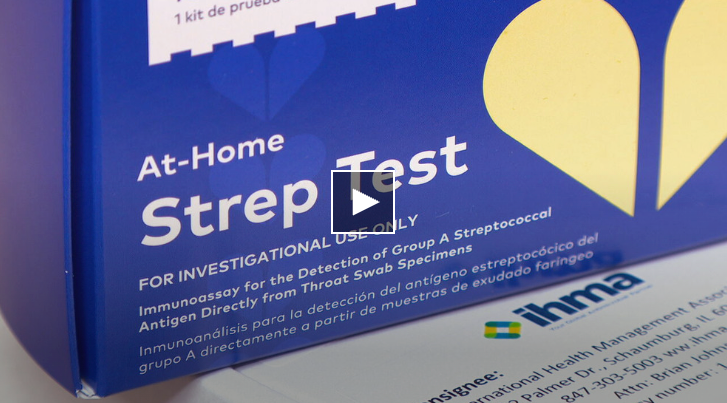
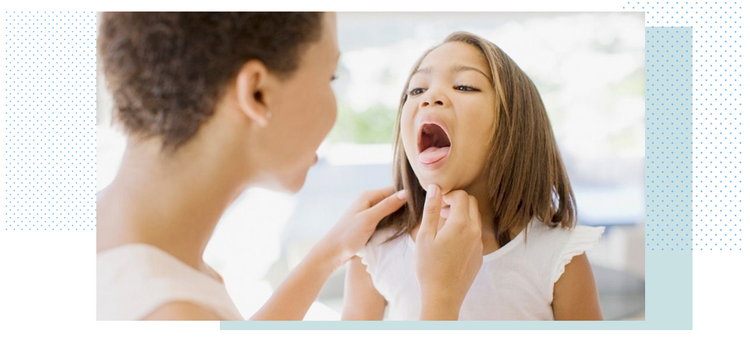
At the forefront of home healthcare, Checkable is developing the first FDA-approved at-home strep test. Paired with a proprietary digital telemedicine platform to instantly connect consumers with healthcare professionals, you can skip the doctor's office and start treatment fast, right from the comforts of your home. http://www.testforstrep.com
Full Transcript:
0:00:01.1 S1: Hello and welcome to the We podcast. My name is Patty Post, and I am Melissa Brant, and our guest today is Dr. Richard Conlen, an OBGYN out of Boca Raton Florida. And what did you think about this podcast? I was actually really nervous going in because any time you have a conversation with a doctor at that level, how intimidating and to ask the wrong question or sound stupid, I was actually blown away of what we covered today, and I walked away going, Oh my gosh, I get it, and I understand my body better. And now I can feel like, Oh, I can go in and ask the right questions, so I was very impressed. Yeah, it's interesting that you only think of an OBGYN walking in, Okay, I'm gonna get my PAP. When you have babies, all of the times that you see them, and then you have your postpartum visit and then you don't really check in with your OB-GYN, but he got into so many different things from cervical cancer to hormones to preeclampsia... Actually, I'm not saying it right, he's corrected me, but pelvic floor trauma after we have kids, and he was very approachable. And I loved it too, because sometimes it's uncomfortable to talk about those things as a woman on how you're feeling or what you experienced Down Under and it was great, and it was a breath of fresh air, and it really...
0:01:34.5 S1: It was informative. Something that I took away was, when you go in to see a OBGYN, you don't have to necessarily get an exam, if you have symptoms or signs that are going on with your body, you should bring them to them because there's so many lab tests that can be done or blood tests that can be done, go to the lab, they interpret the results, and then there is a course of action that you take; a treatment plan per se. Right, and I think one thing that I took away was, Don't wait, if there is something that your gut is telling you that's not feeling good, or you just have a question... There's no such thing as a dumb question. And time is of the essence, and there's ways to make you feel better or get better, and he even mentioned some time sensitive things that we need to be cautious about as women and if you wait too long, it could be your life. So I thought it was really, really powerful. Yeah, once you actually get symptoms, it's too late, so that's why screening is so important, especially with HPV... Exactly, and just being in tune with your body.
0:02:52.7 S1: I hope you get a lot out of this episode with Dr. Richard Conlen. So let's get into the interview. Hey, this is the Wellness Essentials podcast. WE for sure, the WE Podcast is all thing, health and wellness, a place where women like you can come to be their authentic self and be a part of a community that supports them in their health during and every stage of life. This is the podcast for engaging Health and Wellness entertainment with actionable steps you can take into your everyday life. No topic is off limits when it comes to health and women's lifestyle. Let's face it, being a woman comes with all sorts of fun, here, real conversations and teachings from experts and everyday women who have been in your shoes, and it inspired to make things happen and have the tools to do so. This is the WE podcast. Dr. Conlen, do you mind giving your background and how many years you've been in practice, and tell us about your practice and your patient population.
0:04:16.2 S2: Sure. My name is Dr. Richard Conlen, I'm practicing in Boca Raton, Florida, where I practiced for over 35 years, I'm a practicing OB-GYN, although I have stopped delivering, I still do early prenatal care, and I do a fair amount of gynecological surgery, including robotic surgery in office, minimally invasive. Basically, everything that is done gynecologically. I do some specialized hormonal replacement therapy, and I am a referral center for many recurring chronic problems with regards to women's vaginal area, chronic pain, heavy bleeding. I'm also on the Miller School of Medicine’s faculty as an associate professor, and I do teach over at FAU to their pre-med students and the residents at Boca Regional Hospital.
0:05:16.8 S1: Impressive. You don't let any grass grow under your feet, as my grandma would say.
0:05:23.7 S2: You gotta keep moving otherwise they catch up with you.
0:05:28.1 S1: Yes they do. You mentioned chronic conditions. Can you expand on that? Chronic conditions that women can have?
0:05:37.1 S2: Well, probably the most common one is chronic pelvic pain that I see, and this can start out as menstrual cramps in the teenage years, and what they end up doing is they start labeling patients with endometriosis, and to tell you the truth... if I was to do a laparoscopy where I take a look inside and I took 10 people, seven of them would have endometriosis, so endometriosis can be deep in the pelvis, it can be superficial, you can have a ton of it and have absolutely no symptoms and you can have a minimal amount of lesions and have a lot of pain. So it depends, particularly on where it is, so that's a fun thing. As women get older, then we get into child-bearing years, and then most of my practice at that particular time has to do with initiating prenatal care and then referring them out to the specialist, and then if they're not getting pregnant, we do some evaluation to see why they're not getting pregnant, I have to consider that in the overall picture, 40% is men and 50, 60% is women, so rather than getting into that, it can be either side, both sides can have problems.
0:06:58.3 S2: Now, women usually think of their cycles being 30 days, well, what they don't know is that men’s cycle is usually about 90 days, so you can use that to your advantage... Well, you're just cycling today; tell your husband. So the purpose being is that when you do a sperm analysis on men, if you get a normal one then that settles it, but if you get an abnormal one, it doesn't mean that there's a problem, it just means that it could be at the two ends of the curve. And couples, it's a very nerve-wracking thing when you think that you can't get pregnant. Most people can if they just relax. I tell people, and I've been telling people for 30 years, and I'm quite successful at it, you need to relax. Stop thinking about it. Try to have as much fun as you can. And whatever you do, you never call your husband at work and say, “This is the night I’m ovulating, you better be home on time!” 'cause they're gonna go, Oh no. Okay, so no, never do that. After that, it's just routine, women's care, and of course, we hope we don't find anything bad along the way. You get into the fourth decade, it turns out to be some perimenopausal symptomatology, Hormones tend to fluctuate up and down throughout the month, and...
0:08:27.5 S2: So you deal with that. Most of that is transit, I find that women have a little fluctuation around 40, and it can last for six months and then everything evens out. I don't know if it's because of children, the kids are growing up, they're in school, the stresses of life, but whatever. Later on and you get into the 50s, it's more menopausal, you can start having heavier bleeding and we treat that. No longer do women have to have hysterectomies because of heavy bleeding. We do ablation, which I've been doing for 15 years. It works very well. Really? Yeah, it's a great product. It's an outpatient, it's simple, has minimal complications, and it can stop your period but doesn't affect the hormones. So that works very nicely. Of course, unfortunately, during all these years, you do run into some severe problems, some malignancies, we keep a good track on people with abnormal Pap smears, human papillomavirus, and of course, we screen people have the histories of ovarian disease in their family very carefully. So that's kind of an overview.
0:09:43.0 S1: Interesting. You mentioned HPV. At what time should you be routinely tested for HPV?
0:09:53.2 S2: Okay, so that's a very controversial issue. And there's a lot of information that's floating around about human papillomavirus. The first thing we should do... Now, is there's over 100 different strains of HPV. And it used to be that we were concerned about nine, 11, 16 to 18. Nine and 11 usually venereal growth on the outside, whether it be your fingers for young kids, or growths on the outside of the women's genitalia, the 16, 18 was originally associated with cervical disease precancerous lesions, cervical cancer, but what we've learned now is that there are several other strains 32, 54. There's always some changes. I think as we all realize after this past year and a half, we don't know much about viruses and we don't understand how they act, and we have to be looking for trouble. At the present time, they recommend to start doing pap smears and HPV around 20, 21. I don't really believe that. I believe that it has to do with the patient. If the young lady has had multiple partners throughout her life then she should be screened earlier, if she's a victim of trauma, then they should be followed very carefully, so multiple partners, increased risk factors.
0:11:18.7 S2: All of that has to be taken into consideration, and I believe that you should have HPV screening in addition to cytology. Otherwise called co-testing. Just doing HPV is not gonna do the trick. You need to make sure that the HPV has not influenced the cells on the cervix or the vaginal wall, you can get at both places, and that should continue throughout the lifetime. Now, they're starting to tell people in their 50s, you don’t need a pap smear anymore, well, that's when you're gonna have trouble, this is when your immune system starts to decrease, the virus didn't go away, it’s just sitting there waiting. So it's not going away. You need to watch people as they get older more carefully... Not less carefully.
0:12:10.7 S1: I was under the assumption that the virus went dormant or our body shed it after we gave birth, is that something that happens?32
0:12:20.8 S2: No. What they're talking about there is young women in their 20s, if they get an early cervical lesion such as mild dysplasia with HPV because they're young, and their immune system is so vigorous that they will suppress the virus and it can become dormant and get the viral levels can decrease quite a bit, and it can lie there for awhile... So that's what happens, you get infected in your 20s, your natural immune system suppresses it, and then come in your 40s, it starts to bloom, and that's when you start having trouble and then it takes five, six, seven years. And come your 50s is where you're running into dysplasia.
0:13:05.2 S1: And what is dysplasia?
0:13:06.8 S2: Dysplasia is precancerous lesions. I like to explain dysplasia as everybody understands termites. So if you have termites in your attic, that would be mild dysplasia. If you have termites in your attic and the second floor, that would be in situ, moderate dysplasia. If you have termites in all three levels, that would be severe dysplasia or high grade... Okay, Your house sits on a cement slab, well, your cells sit on a cement slab, the last barrier, and that's called the basement membrane. As long as those dysplastic cells do not go below the basement or past the slab, you're okay. If it goes all the way through the house, down to the cement, we call that carcinoma in situ, and all of that is curable by taking a LEEP cone biopsy and just removing that area. Once it goes below the cement, the basement membrane, it becomes invasive and that could be more severe. It is more severe.
0:14:21.8 S1: And then is that where you get uterine cancer or...
0:14:26.0 S2: That's where you get cervical cancer, and cervical cancer is a bad boy, and it goes below seven millimeters, then you can fight that for the rest of your life, and in many cases, it's going to be bad for you in the long run. Many people don't survive.
0:14:43.6 S1: And are there signs or symptoms?
0:14:46.6 S2: Bleeding after intercourse, bleeding for no reason at all, usually pain is the very late onset. Really? Yeah, so the key thing here is to find it early, if you get pap smears even every two years, you have a five-year window in most cases, to catch something that can be fixed very easily. If you let that go by... No good. Uterine cancer is cancer of the body of the uterus, and that is also, there's a large leeway there, because that's not severe until the cancer goes actually 50% of the wall, it's all simply cured with hysterectomy.
0:15:33.8 S1: So you could go for years without a pap and it is actually detrimental. If you have HPV, that is invasive, 'cause insurance companies now are saying, Oh, you don't need one after 40 until every five years. I know. What's up with that?
0:15:53.9 S2: Well, not something that I wanna get into on a podcast, but... Well, what do you think it's all about? It's about the money. It’s about the money. So they have studies that show that it doesn't make any difference, but as I said, and I presented my case at the FDA, I was about some testing, I was on the panel that did that, and I said to them, and I said you know, and these academics would get up there and say, “Well, you know, the statistics show this and that”, and I turned to them, I said, “Have you ever sat across from someone and given them very bad news, 'cause they're not interested in the statistics, they're only interested in themselves.” And sitting there telling them, “Well, you know statistically, you probably shouldn't have got that.” Well, that's a good way to have somebody crawl over your desk with a knife... That's not it. So as a practicing physician and someone who's dealt with women's care for over 35 years, I'm not interested in the statistics, I'm interested in the people that sit in front of me and trying to keep that down. The pap smear was a wonderful invention and decreased the amount of cervical cancer, significantly across the board, but we still lose 14,000 women to cervical cancer every year.
0:17:20.6 S2: Wow. Because they don't get screened. And that's why I promote self-testing... 14,000.
0:17:28.7 S1: That is a significant number.
0:17:31.1 S2: How significant is that? By the time we're done with this podcast, somebody would have died. Wow. Yeah, and they think that's okay. And then this plateau, now it used to be much, much higher. And that has plateaued, and that's where it is, and the only way that we're gonna get that down is to get everybody screened, but that's like trying to get everybody vaccinated.
0:17:56.0 S1: So here's something that being in medical devices, I was around a lot of devices that were for the prostate, or urethra strictures for men, and there was a lot of investment dollars put behind them, and then when we went over to pelvic health and gynecological health, the numbers decreased drastically. And from your experience, do you find that that's true? That the number of research dollars for women versus men and our reproductive organs is not as high as men?
0:18:36.6 S2: I don't know that I can really comment on that. Honestly, I will tell you that as a rule, women run healthcare. Okay. Yes. Breast cancer and screening and obstetrics and everything else, it's all up to you. Do I believe that? I don't know. But I know that we've made big strides in breast cancer, we try very hard with ovarian cancer. Uterine cancer, we understand it, as long as people will come in; cervical cancer we can do very well with as long as women come in. Now, having said that, there's always a small percentage of people that get a very severe type of disease that we don't do very well with, but as a majority, if we can see them, we can screen them, we can help them.
0:19:28.9 S1: So this is a public service announcement to go get your pap or your mammogram, if you haven't done it yet... Oh, absolutely.
0:19:37.3 S2: Yeah. There's no excuse. I mean especially in October, it was... October is National breast screening, and you can get a mammogram for 50 bucks. You can’t get a manicure for 50 bucks, right?
0:19:49.8 S1: Yeah, very true. Okay. Okay, so let's switch gears. Well, I was thinking maybe hormonal therapy for women, there are a lot of conversations, we were just out with some friends yesterday in talks of... What do we do when we're in our 40s and 50s? Our hormones are imbalanced. There's all different things that we could do. What are the ways that you are seeing or recommending for women in their 40s and 50s in terms of solutions for them and their hormonal balance...
0:20:27.8 S2: Okay, when it comes to hormonal imbalance, the one thing you have to take into consideration here is quality of life. Some people suffer. Some people suffer a lot. Some people don't get any symptoms, okay, so for those that have considerable symptoms, sooner or later are going to have to make a decision with regards to hormones versus non-hormones. If you do the herbs and the supplements, I encourage you to change the brand every three months, because they don't have the bioactivity of regular pharmaceuticals, so you have to switch from brand to brand. And for a lot of people that will hold them to mild symptoms or in early menopause or perimenopause.
0:21:18.9 S1: The team at Checkable Medical is famously fussy about what goes into their bodies, optimal health at every stage, in every age is key to living a life you love, those better supplements, we Superior ingredients in simple, easy-to absorb formats that fit into your daily life, feel your best would Checkable Wellness. If you're ready to get started, check out, CheckableWellness.com for more details. Your healthcare begins at home.
0:21:49.8 S2: If the symptoms are bad enough that it's ruining your life, then you have to consider hormone replacement therapy or you should. And with that, you need to be counseled as to the overall risk involved with regards to breast cancer, and all the other side effects. Now, women have a risk of developing breast cancer one in eight. Everybody has to take that into consideration whether you're BRACA tested or not, it's one in eight across the board, so you do the best you can to try and find it early, I hope you do well. And most women will, with regards to quality of life and hormones. Let's talk about hormones, there's three estrogens that are made... I like to explain it as high test, medium grade and low grade. Nobody gives the low grade, that's estrone, it's a weak, but insidious and dangerous estrogen. Your body runs on 80% medium-grade estriol, and 20% high-test estradiol. Most of the traditional hormone replacement therapy is estradiol. They're giving you high-test, and then you should take some progesterone with it. It’s progesterone, not progestogen. Progestogen is the synthetic progesterone, and that is associated with breast problems.
0:23:20.4 S1: Oh, wow. Will a doctor prescribe that?
0:23:24.0 S2: Some people do. Progestogens are what’s in birth control pills. It doesn't seem to make a difference, but nobody really knows. Okay. Once you get older, it is progesterone, prometrium, that type of thing. Now, you also need testosterone. So for many years when I was first out in practice and I would see people... give them the estrogen and they come back in a month later and I say, How do you feel? They go “Um, I feel ok”. Okay. But they're blah. Then I started adding testosterone and they'd come back and say, “Yep, I’m back! I feel good.” Now, many think that testosterone has to do with sexual activity. It really doesn't. Once the body is balanced, the body does what the body does, and sexual activity is part of what we do, so once you’re balanced, you feel better, but testosterone brings back the clarity, gets rid of the brain fog. But it also has to work together with your thyroid and your adrenal, so when I approach people for hormone replacement therapy, I evaluate all of them, everything has to be clicking.
0:24:33.0 S1: If we were to go to our doctor to ask for a panel, what's like a cocktail panel that we should ask for to ensure that we are getting the right tests done.
0:24:43.9 S2: I would do an FSH, which is called follicle-stimulating hormone. This is the brain telling the ovaries to get going, the higher that number, the more you're into menopause. I would get an estradiol level, I would get a testosterone level, you can get free and total, but either one, it's going to tell you the story. Progesterone has a very short half life so they always include it in the panel, but it really doesn't have a significant effect. Some people like endocrinologists will get LH and all of these other sub-factors, but you're not really making that if you’re menopausal because you're not ovulating regularly. I would get those. I would get a thyroid profile to make sure your thyroid is working properly. The thyroid is the motor of the endocrine system, if that's not working, nothing's working. So that's what I would do. That's what I do.
0:25:36.6 S1: That's exactly what you do for your patients. Right, okay. And then they come back, you read it, you analyze it, and then you make a recommendation, what's the treatment?
0:25:48.9 S2: I give them a choice: Do you wanna do traditional? You wanna do bio-identical, which can be delivered as rapid-dissolve tablets, topical cream, drops, or we can do pellets, which are testosterone pellets. Can you see that?
0:26:04.2 S1: Oh yeah, yes.
0:26:05.7 S2: A little pellet in there, yeah, and I put it in your backside under the skin, and it encapsulates and then your body draws from that because testosterone metabolizes down into estradiol and the body kind of self-regulates. Not exactly like that. Still take the progesterone. So those are the three choices. Financially, insurance pays for the traditional, it doesn't necessarily pay for the bio-identical, which is a combination, so that we balance for you. So what happens is, everybody's an individual, I prefer to get blood work after they're on it for a while and they feel good to make sure they're not getting too much. I want people to get the smallest amount to give them the maximum amount of relief. And I do that for the bio-identical as well as the pellets.
0:27:02.6 S1: Very helpful, and it's super helpful. Is there any transdermal patches that deliver... Oh, there are.
0:27:10.2 S2: I should have mentioned too, that I don't give any pills, my rapid-dissolve tablets dissolve in the mouth, but I don't like pills because that goes through your liver, and that changes the coagulation profile as well as your lipid profile. So if I give the traditional approach, I'd give it as a patch.
0:27:29.2 S1: Oh, interesting, I like that. Let’s switch gears. Now, I wanna talk about bacterial vaginitis or is it bacterial vaginosis? BV. We can just call it BV.
0:27:45.5 S2: Okay. This is a very common infection, and although it can be associated with sexual partners, it really isn't considered a sexually transmitted disease, but it is recurrent and you do pass it back and forth between the partners. Okay, and what it is, it reflects a change in the environment of the vagina. The vagina has to have certain bacteria and those bacteria work together in the microbiome, so to speak, we’ll use fancy terms here, in check and in balance so that it takes care of itself. We like to refer to the vagina as a self-cleaning oven. Left to itself, it will come back into balance, but when you introduce sexual activity, you introduce virions, viruses, bacteria, jellies, all sorts of things, okay. And that tends to change it. When someone has growth of certain types of bacteria, it promotes the recurrence of bacterial vaginosis, such as A. vaginalis, these are all facultative anaerobes that can be in there, or megasphaera, there’s two types. One is associated with trichomonas, one is associated with BV. So all of these things should be looked at carefully to see what's going on. The telltale test where people come in, is they get a certain odor, it's a strong odor, it's a fishy odor. And this occurs with intercourse because the male is alkaline and she is basic and when they mix they give off that odor when that's present. And also if you get it recurrently, it gets caught in a mucus development that sticks on the wall.
0:29:44.7 S2: I like to tell people, if you've ever...probably not now, but maybe when you were all in college and things, and we wake up in the morning, we didn’t brush or the night before…we didn’t know where we were the night before…and you have that stuff all over your teeth. Right, that's what happens. And the bacteria harbors in that, so that could be how you’ll remember that one, won’t you? And what happens is that harbors in the vagina, so one or two treatments of medication isn't going to do it, which means you have to have recurrent antibacterial treatment and get rid of all the other associated bacteria
0:30:24.6 S1: And... Is that an antibiotic? Oral antibiotic
0:30:27.6 S2: Can be, sometimes it can be a cream, they have new medicines that are out, that come as drinks, you take it once and you're set, they have new medications that are coming on, even for candidiasis, remember there's several different types of Candida, one is easily treated with the cream and one isn’t. Now they have medicines, it's a one-time dose to take care of, so we are making progress in this area, but you just can't shoot from the hip, you have to have some testing to find out exactly where you are.
0:31:01.9 S1: And running to CVS to grab Monistat if you're douching a lot.
0:31:09.4 S2: We don't douche. Don't douche
0:31:11.4 S1: No douches. We agree.
0:31:15.3 S2: That's over. I don’t think that was a good idea.
0:31:20.8 S1: Because it takes a good bacteria away...
0:31:24.1 S2: It just disturbs everything. Yeah, And it takes time to rebuild it. It will rebuild. Now, as you get older and you’re not making as much estrogen on your own, the vaginal area gets dryer, it presents a whole different set of bacteria and problems associated with that.
0:31:44.2 S1: It's like a desert.
0:31:46.2 S2: Not so much as a desert. Remember, your skin is always exfoliating, right? Yeah, so is the vagina, so you don't have that discharge coming out all the time, it's sitting in there. And we call that desquamative vaginitis, so they sit there and that makes a focus for infection.
0:32:10.3 S1: And so do you take an antibiotic for that as well?
0:32:14.7 S2: No, most of the time we use some estrogen vaginal cream periodically a couple times a week, just to get the moisture back flowing, not enough to really be a risk. I give a lot of people that small amount of estrogen infrequently, but on a regular basis who have had breast cancer and things like that.
0:32:35.5 S1: If you feel like you have this recurring yeast infection, having a test... what if you don't have health insurance and you wanna test from home, you have a product that's justgettested.org, and you run a panel of tests, can you tell us what that panel is because there could be listeners that wanna order it...
0:33:01.5 S2: Yeah, there's three of them that we like to do, there's an STD panel, but if you're pretty sure you don't fall in that realm and you're just getting recurrent vaginitis, then we would test for BV. We would also test for E. Coli, some of the bacteria that are currently present down there, that can become a problem once the environment gets out of balance, and we would test for megasphaera and A. vaginalis, all of it, so that we get a nice picture of what's going on. I still have patients who come into my office at all ages and say, Well, I have a yeast infection, and we do culture and it's not a yeast infection, it's a bacterial infection. So not every irritation, itchiness, discharge or things like that is yeast, but that's all we knew about 30 years ago. So that's stuck with everybody.
0:34:01.0 S1: So I shouldn't call it a yeast infection.
0:34:03.4 S2: Well, those people come in and say, I've got something going on down here. So if you're at home and you have something going on and you don't wanna go to the doctor or you can't get in or something like that, then it's better to start doing the kits that are available out there, your kit, my kit, all of them that are available out there, so that you can get treated. It's easy, you'll have the kit in two days, do the kit, send it in, you get the results back in 36-48 hours.
0:34:35.3 S1: It seems like with the light of what we've talked about today, you don't need the pelvic exam to be diagnosed, it actually is lab results, and that's what you use to determine the diagnosis...
0:34:49.7 S2: Right, if you have a problem, abnormal bleeding, post-coital bleeding, pelvic pain, anything that's going on that you feel is anatomically different than at this particular point, there is no way you can do it at home, however, through telemedicine platform, the appropriate test can be ordered because we'll do an ultrasound anyway, no matter what.
0:35:15.1 S1: When you have preeclampsia and you have had pelvic floor trauma, we have a friend that is going through physical therapy, and every time she ran or sneezed, she would wet herself. So what happened was, everyone says, Oh, do kegels, do kegels, you have to tighten it up... Well, she had the opposite where she was always tight and she wasn't able to relax, and so she's now going through some physical therapy where they are teaching her how to relax, and I think there's not a lot of awareness around that, and we end up just living with it. And I think because of the slings and meshes of what happened 10 years ago, and we're very nervous of that, or we've seen our mothers go through problems with that, that now we're kind of in this gray area. Well, okay, should we just live with it and wonder, what do you recommend to your patients?
0:36:19.7 S2: I do pelvic floor here in my office a lot. And I have to tell you, and I also did the slings and I did the surgeries, and I've done all that, and I did not believe that the pelvic floor rehab was going to do anything. Well, I was wrong. Very wrong. Okay, and it works very well. Okay, so try to explain this to people, they're not looking at me: the pelvis is a bowl. It's a bowl made up of muscles, and when you breathe like your diaphragm, it goes up and down as time goes on. Those muscles get weak, either due to the lack of estrogen, trauma, children, whatever. And they're not stimulated. So with the pelvic floor, they stimulate those muscles to come back to life and they allow you to realize what muscles you should be stimulating to pull that up. I had a professor over an FAU; a pretty interesting case, she developed a really total incontinence, and her career is over. Yeah, so we ended up doing a pelvic floor and took her 10 weeks of treatment. And she’s back to work. Now, I don't know how long it will last 'cause you really don't know the etiology that causes it but there is hope.
0:37:44.5 S2: I have a sign in my office, it says, “Sometimes I lag so hard, tears run down my leg,” and it's true, and it can be incapacitating to women. It's a big deal. It is a very big deal. I don't know where the pre-eclampsia came from with the pelvic floor. Is she young? Old?.
0:38:04.3 S1: She's in her mid-40s, she has a couple of children...
0:38:07.5 S2: Yeah, so she should do the pelvic rehab, he should find it, she can find it in a medical center nearby, she... Or you could call a company called Consortia, and that's who I used and they send a tech out and it works very well. I would say with my experience in the past couple of years, we're at 85%.
0:38:28.2 S1: Really? That's very good. Yeah, very good. Cool, thank you for that. Yeah, well, I think this was an information-packed session with you, Dr. C, thank you so much. You're welcome, our time with the Doc is always valuable.
0:38:49.3 S2: No problem. You want me to come back for questions or whatever you wanna do, you know I'm... I'll do it.
0:38:55.3 S1: Well you're the best thank you Dr Conlen it was very nice people with you
0:38:59.9 S2: And good luck, have a nice day!
0:39:01.6 S1: Thank you, too! We hope you enjoyed this episode of The WE podcast as much as that if you want more wellness goodies, head over to the wellness essentials Podcast dot com or show notes, links and resources mentioned in today's podcast remember to subscribe on your favorite podcast platform to get all the wellness details as soon as they are released. Cheers to living your healthiest and happiest life.
Life is too short to sit in a doctor’s office
Sign up for our weekly newsletter and get valuable healthcare tips and tricks in your inbox!
Sign up now and unsubscribe anytime.
- Choosing a selection results in a full page refresh.
- Press the space key then arrow keys to make a selection.