You asked; we answered. You’ve likely had a case of strep throat before as a kid, or you know someone who has. It’s one of the most common infections, especially for school-aged children between 5-15. It's estimated that millions of people are diagnosed with strep throat in the United States annually. Strep throat is a bacterial infection caused by a bacterium belonging to Group A beta-hemolytic Streptococcus (GAS), Strep for short.
Generally speaking, strep throat affects children more frequently than adults. Approximately three out of every ten cases of sore throat is classified as a strep throat infection. In this article, we’ll answer your most frequently asked questions about strep throat.
Who is at risk for catching strep throat?
Strep throat is one of the most common bacterial infections and is highly contagious. Anyone exposed to it can get it, but school-aged children tend to get strep throat more frequently than adults and are the most vulnerable to exposure. To no surprise, parents of school-age children are also more likely to get strep throat. It seems that sharing crayons isn’t all that gets passed around in school.
Compared to younger children (less than five years old), kids aged 5-15 years old have a higher risk of strep throat infection (24% risk for younger children vs 37% risk for school-aged children). Adults are the least affected age group, with a risk of getting strep throat ranging between 5-15%. Strep throat infections are generally more common in late winter and early spring.
How can I tell the difference between strep throat and other causes of sore throat?
A sore throat is the most common symptom in many illnesses, so it is important to look at all the symptoms and test for it. From environmental irritants, allergies, having the flu or the common cold, and even just sleeping with your mouth open can all cause a sore throat.
Despite the fact that strep throat is the most common bacterial cause of sore throat, the most common causes of sore throat, in general, are viruses. That's why strep throat can sometimes be misdiagnosed as tonsillitis or viral infections, like infectious mononucleosis or hand-foot-and-mouth disease.
The seasonality (late winter and spring) and the symptoms can help in distinguishing these infections from true Strep throat infections. Strep throat is characterized by having a rapid onset of symptoms, high fever (over 100°F), and intensely red inflamed tonsils and throat with white dots.
A virus with strep-like symptoms, infectious mononucleosis, can also be the culprit. This is most common among teenagers and young adults (college students seem especially susceptible to a mono infection) and causes more fatigue and greater swelling of the lymph nodes in the neck (cervical lymphadenopathy) than a strep infection.
Hand-foot-and-mouth disease is characterized by painful oral lesions and rash in the hands and feet and is more common in babies and young children under five. Also highly contagious, this virus typically resolves itself with time.
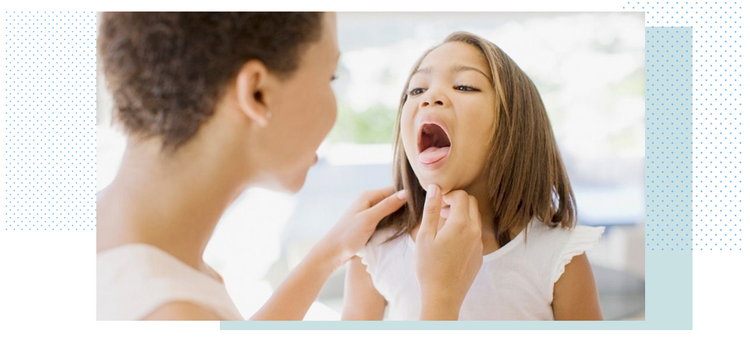
How to diagnose strep throat?
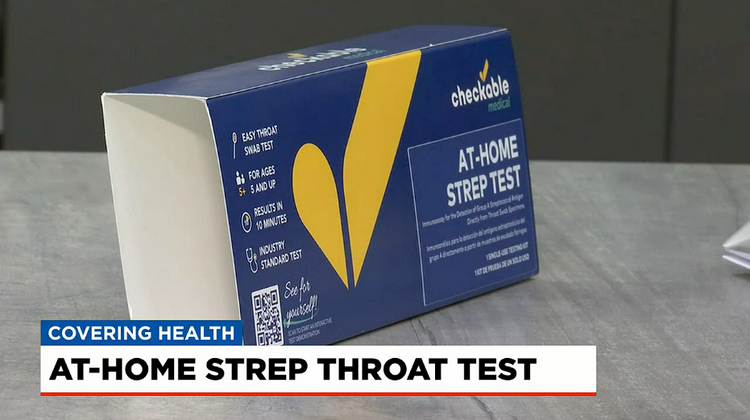
If all the symptoms of strep are showing, it is important to test for strep, as it is highly contagious and can get more serious if left untreated. Strep throat is diagnosed using rapid antigen detection testing (RADT). Either performed at home by your doctor, a simple swab of the throat will review the results of the test to determine if strep bacteria are present. If the rapid test comes back negative, but strep throat is still suspected, your doctor may take a throat culture that goes to a lab for further testing. It is a good idea to keep a few at-home strep tests on hand for fast and accurate results in minutes.
If you have a positive case of strep, the doctor will prescribe a course of antibiotics. After starting antibiotics, you should start to feel better within a day or two. It’s important to finish your course of medication completely so that the infection doesn’t return.
Those who test positive but don’t show symptoms are called carriers. Usually, those who are asymptomatic carriers are generally not prescribed antibiotics. If symptoms do develop, it’s important to let your doctor know.
Is a tonsillectomy recommended for recurrent strep throat infections?
A tonsillectomy (removing the tonsils) is an invasive procedure and should be considered only after careful assessment and discussion with your doctor. Children typically bounce back from a tonsillectomy much quicker and easier than adults; maybe it's the ice cream they get to eat.
You may be a candidate for a tonsillectomy if you have a certain number of recurring strep throat infections over the course of a year. Your doctor will determine how many infections are too many, warranting surgery. If you develop an abscess on your tonsils or throat, this may make you eligible for a tonsillectomy as well.
Those who are allergic to any medication used to treat strep throat infections are also good candidates for a tonsillectomy. Strep throat can knock you down, but not out. A quick diagnosis and a course of antibiotics will have you feeling better in no time. If you are still unsure, check out our step-by-step guide for diagnosing strep.
Life is too short to sit in a doctor’s office
Sign up for our weekly newsletter and get valuable healthcare tips and tricks in your inbox!
Sign up now and unsubscribe anytime.
- Choosing a selection results in a full page refresh.
- Press the space key then arrow keys to make a selection.