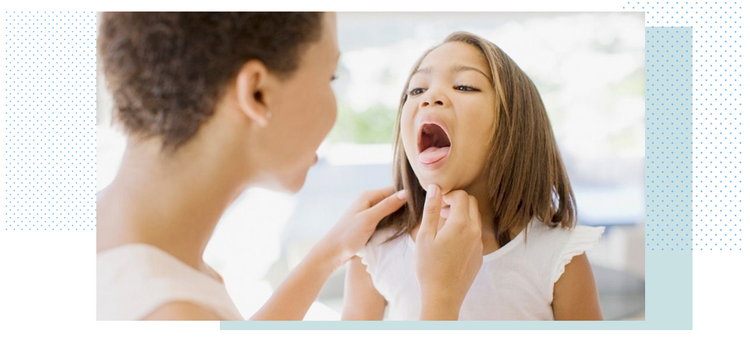
Strep throat is one of the most prevalent bacterial infections among children. It's estimated that every year about a quarter of school-aged children between 5 and 19 years get infected with strep throat. If you’re a parent, those numbers are no surprise to you. It seems like nearly every parent has dealt with strep throat before either in their own childhood or with their kids. It peaks with the school year and colder weather, and spreads easily in schools and daycares.
Since strep throat is due to bacteria, Streptococcus pyogenes, it can be treated with simple antibiotics. Although it can resolve on its own without medications, it’s important to start antibiotics as soon as you have a confirmed case. Waiting too long or forgoing antibiotics completely can lead to serious complications that can affect the heart and kidneys.
With most strep throat infections, the symptoms usually start to improve markedly after three to four days, even without treatment. It’s still highly recommended to start antibiotic therapy as soon as possible because medication decreases the amount of time it takes for symptoms to improve. Symptoms generally start to improve after only one to two days once antibiotics have been started.
Additionally, antibiotics are primarily given because they decrease the rate of strep throat complications. One study showed that giving penicillin to strep throat patients reduced the rate of Rheumatic fever (a serious strep throat heart complication) by twofold. In addition to penicillin, cephalosporins (a family of antibiotics) can also be used to treat strep throat infections. Compared to penicillin, cephalosporins work faster than penicillin in terms of decreasing the severity of fever and sore throat that accompany strep throat infection.
What is Antibiotic Resistance?
According to the CDC, antimicrobial resistance happens when germs like bacteria and fungi develop the ability to defeat the drugs designed to kill them. That means the germs are not killed and continue to grow. Resistant infections can be difficult, and sometimes impossible, to treat.
Antimicrobial resistance is an urgent global public health threat, killing at least 1.27 million people worldwide and associated with nearly 5 million deaths in 2019. In the U.S., more than 2.8 million antimicrobial-resistant infections occur each year. More than 35,000 people die as a result, according to CDC’s 2019 Antibiotic Resistance (AR) Threats Report. When Clostridioides difficile—a bacterium that is not typically resistant but can cause deadly diarrhea and is associated with antimicrobial use—is added to these, the U.S. toll of all the threats in the report exceeds 3 million infections and 48,000 deaths.
How does antibiotic resistance happen?
Antibiotics are heavily prescribed for conditions that don't require them. For instance, doctors are easily prescribing meds for sore throats that are caused by a viral infection like the cold or flu. Antibiotics can not kill a virus; they are only necessary for bacterial infections, including strep throat.
The studies that support treating strep throat with antibiotics are numerous; however there is a growing counterargument against using antibiotics to treat Strep throat. Despite the body of evidence showing that antibiotics decrease the rate of complications, some argue that these complications might arise without showing symptoms of strep throat to treat in the first place. For Rheumatic fever for example, some argue that roughly 60-75% of Rheumatic fever cases are preceded by sore throat and that antibiotic therapy will only prevent a few cases.
Some reports estimate that the rate of Rheumatic fever due to strep throat has been in decline even before starting the routine practice of treating strep throat with antibiotics. Furthermore, most patients presenting with Strep throat symptoms actually have viral infections, and any Group A Strep organisms detected are because they are in fact carriers for Strep throat and have a low risk for strep throat complications.
Additionally, using antibiotics on a large scale to treat strep throat infections might lead to rare but rather serious complications like anaphylaxis, which is a severe allergic reaction to antibiotics. Increasing the use of antibiotics to treat Strep throat infections also increases the risk of antibiotic resistance. For example, the number of Group A Strep bacteria that macrolides (a family of antibiotics) are effective against is declining in countries with high use of macrolides to treat Strep throat infections.
The Bottom Line
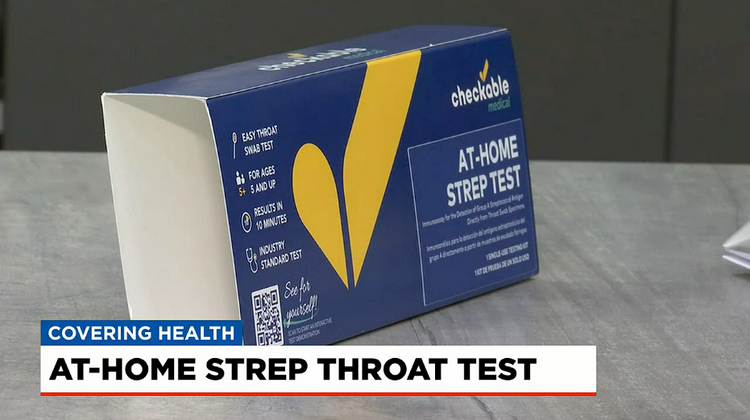
With all that being said, we feel the best course of action is first to confirm that your child’s sore throat is actually strep. Keep a few at-home strep throat tests on hand and know for sure what is causing the sore throat. If the strep test is negative, there is no need for antibiotics unless there is some other bacterial infection like a sinus or ear infection. If the test is positive, your doctor should prescribe antibiotics for 7-10 days. You can also sync the at-home tests with Checkable's new telehealth app and connect to a healthcare provider for fast treatment without leaving home.
Life is too short to sit in a doctor’s office
Sign up for our weekly newsletter and get valuable healthcare tips and tricks in your inbox!
Sign up now and unsubscribe anytime.
- Choosing a selection results in a full page refresh.
- Press the space key then arrow keys to make a selection.